Talking about IBS doesn’t have to be uncomfortable or taboo.
Talk to your doctor to better understand your IBS and learn which treatment options are available to help you and your poo!
Why doesn’t everyone experience
IBS in the same way?
Have you ever wondered why more women seem to suffer from IBS than men? Is this a coincidence, or is there some validity behind the observation?
You’re not alone in being curious about this matter. Researchers have conducted numerous studies investigating whether gender influences one’s likelihood of developing IBS. As it turns out, IBS is significantly more common among women compared to men, with 2 to 3 times as many women being diagnosed with the condition than men.1 In other words, for every man with IBS there are at least 2 women.
So, we know that more women have IBS. But do their symptoms differ too? Studies show that both genders experience abdominal pain to a similar extent.2 However, women report more digestive symptoms that are not associated with pain.2 These include bloating, nausea, and constipation, as well as non-digestive symptoms.2 What do we mean by non-digestive symptoms? These are things like migraines and chronic fatigue syndrome.1 Additionally, women’s IBS symptoms change throughout their menstrual cycle, with more frequent and severe symptoms, like loose stools and bloating, occurring during menstruation.1 Of course, this is simply not an issue for men.
What about quality of life? Is that different for women with IBS too? Living with IBS presents many unique, often frustrating, challenges that can affect one’s daily life. That is to say, IBS significantly impacts an individual’s ability to live their life to its fullest. Women with IBS report a lower quality of life than men, resulting in higher levels of fatigue, depression, and anxiety.1 To add to this, women find that IBS has a greater impact on their body image and personal relationships compared to men.1 Now, you may be asking yourself, what is the reason for the increased incidence and impact of IBS among women? While the definitive reason for this gender difference remains elusive, research suggests there are many biological, bacterial, psychological, and social factors at play.
Firstly, men and women are very different, hormonally. Estrogen and progesterone, two of the dominant hormones in women’s health, inhibit smooth muscle in the gut from contracting.1 Without the contraction of these muscles, digested food doesn’t get pushed through the digestive system as quickly, which can result in constipation.
Estrogen also plays an important role in pain perception. Women report more severe, frequent, and long-lasting IBS-related pain than men.1 This could be because estrogen acts as a central nervous system stimulant (i.e. it increases women’s sensitivity to pain).1 Conversely, testosterone, the predominant sex hormone in men, inhibits this pathway, explaining why men report less IBS pain.1 What about bacterial factors? One of the root causes of IBS is a bacterial imbalance in the gut.3 Therefore, differences in gut flora between men and women may explain why women are more commonly and severely affected by IBS than men.4 Gender roles have also been found to influence the manifestation of IBS symptoms. For example, women are generally more anxious about the effects of IBS on their appearance, such as not wanting to look bloated.1 Whereas, men tend to be more affected when their IBS symptoms cause them to feel weak and unable to support their families.1 Finally, men and women differ in their healthcare-seeking behaviours. Typically, women are more likely to visit their primary care provider than men.5,6 This could explain why data shows more women have IBS than men, as perhaps more women are seeking professional, medical care.
Irrespective of gender, it’s important not to feel embarrassed or stigmatized by an IBS diagnosis. If you’re experiencing IBS symptoms, talk to your doctor about all the available treatment options to help restore your gut bacteria, improve your digestive function, and get your symptoms under control.
IBS Doesn’t Rest, Even During a Pandemic
Entering into a global pandemic was a stressful and unusual time for everyone. Many of us had to learn to work from home, travel halted, and in-person socializing became a thing of the past. While most of us have now settled into a “new normal” and the initial stressors of the pandemic have subsided, this may mean you have become complacent about managing your IBS. Being unable to go into the office, or journey far at all, may have minimized your symptoms, creating the illusion that your condition is improving. Consequently, if you’re feeling less burdened by your IBS, you may not be seeking treatment.
So, why is it that the COVID-19 pandemic is causing people to be less proactive about managing their IBS? One reason could be that you’ve adapted to the ‘work from home’ lifestyle. Having easy access to a washroom all day means you can relieve yourself as often as needed, without having to rush off in front of your colleagues when you get the urge. You might be preparing more meals at home, permitting you better control of your diet in avoiding exposure to trigger foods. With many cancelled events and social gatherings, sleep and exercise may have become a higher priority. And, after a year of adjusting to pandemic life, you’re probably less stressed, what with no daily commute, frequent work breaks, and constant access to home comforts.
Another reason you may be putting off seeing a doctor about your IBS is due to a fear of attending in-person appointments. There is, understandably, a heightened anxiety about leaving the house because of the risk of contracting COVID-19, and the doctor’s office is no exception.
Whatever your reasons for not seeking IBS treatment, now’s your chance to reflect and reconsider your position. Why? Untreated IBS can significantly impact your physical and mental health in the long-term. When IBS is insufficiently managed, it can lead to sleep disturbances, such as insomnia, fatigue and lethargy, chronic pain syndromes, and serious mental health conditions, like anxiety and depression.1,2 Not only that, but untreated IBS reduces overall quality of life and productivity levels at work, so it’s really not something to ignore. 2 It’s common for individuals with IBS to suffer in silence, although it doesn’t have to be that way. One study reported 67% of people with IBS experienced symptoms for more than a year before seeing a doctor.3 That’s very significant, given that it can take about 4 years just to receive a definitive IBS diagnosis. 3 While it’s tempting to hide away at home until everything ‘blows over’, there are exceptionally few advantages in doing so. Why not use this time to, instead, focus on improving your health
and well-being? Making the most of your pandemic time to address your health is a great opportunity to try and get your IBS symptoms under control for when life returns to normal.
Let’s consider some practical IBS management activities for you to practice at home. Try eating at regular time intervals, keeping a log of everything you eat and any associated symptoms, exercising regularly, and drinking plenty of fluids.4 You’ll also want to consider taking probiotics, eating probiotic-containing foods (e.g. kimchi, kefir, and kombucha), and talking to your doctor about medications that act on your gut bacteria to help alleviate your IBS symptoms.4 This is because the root cause of IBS is often an imbalance in your gut bacteria. 5 As you can see, at-home management is helpful and necessary, but seeking complementary medical treatment is equally as important. IBS doesn’t rest, even during a pandemic. Make an appointment to discuss IBS treatment options with your doctor today!
Let’s Talk About #2:
Stool Tools for Monitoring IBS
It can be difficult to know what’s considered normal when going to the bathroom. But your stool can tell you a lot about your digestive health and how your IBS is being managed. It’s important to pay attention when something feels – or looks – off because this information can end up being really valuable when talking to your doctor about your IBS.
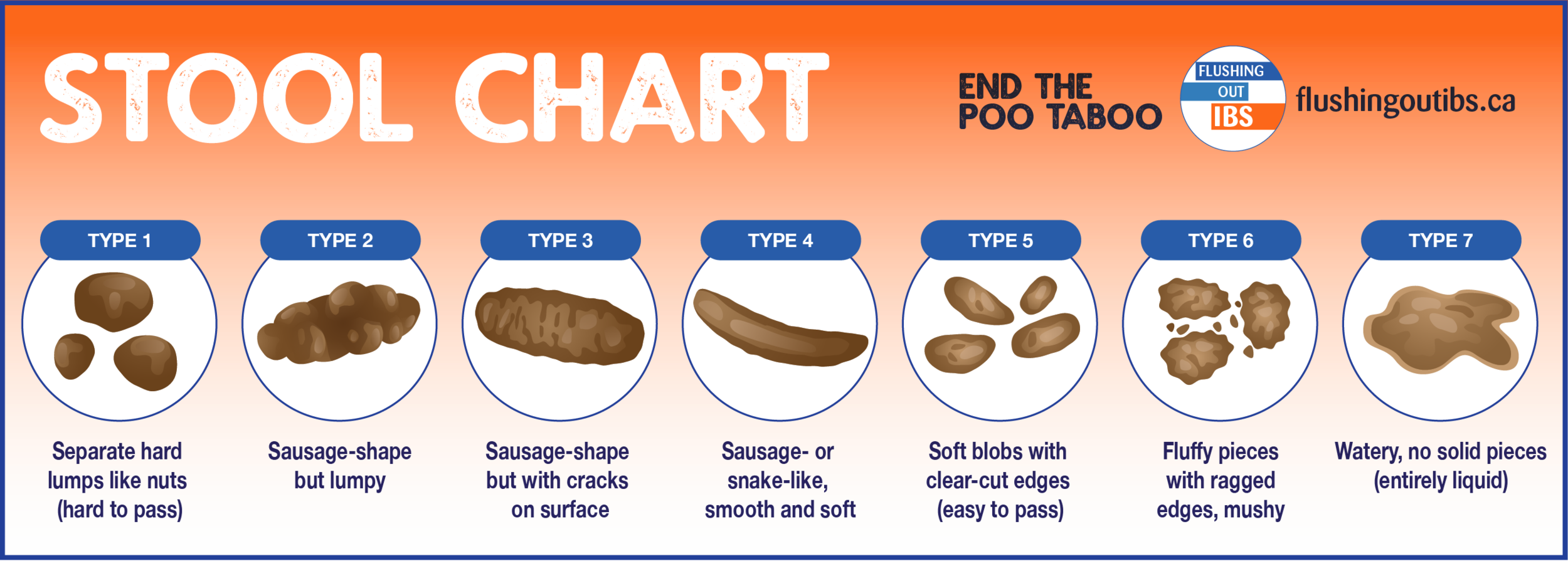
Believe it or not, there’s a useful, practical tool known as the Bristol Stool Chart that can help you determine whether or not your poop is considered ‘normal’. 1,2 The chart is divided into seven different types of stool: the first two are associated with constipation (hard, lumpy stools), the last two with diarrhea (watery stools), and the middle types with healthy bowels. 1,2 As you can see, the ideal type of stool is sausage-shaped and has smooth edges.
It’s important to monitor your stool’s appearance often because this doesn’t just affect which subtype of IBS you get diagnosed with, but also how your doctor will approach treating you.2,4 For example, if you present with looser stools when you first speak to your doctor (e.g. Type 6), you’re more likely to be diagnosed with IBS-D (diarrhea-predominant IBS) and be prescribed treatment to help with this, compared to if you initially present with a Type 1 stool.
Because all IBS diagnostic and management information is self-reported, it can be difficult to know when and how you should be discussing your bowel movements with your doctor. You may not remember how often you’ve experienced abdominal pain, or when you last passed an abnormal stool, unless you’re actively keeping track of this information. This is where tools like the Bristol Stool Chart come in handy. Tracking your daily bowel movements, digestive symptoms, dietary intake, and other potential triggers can be extremely beneficial in helping you determine when you need to take action.4
Stool and symptom tracking can help provide a clear and more complete understanding of IBS symptoms for both you and your doctor.
So, what exactly should you be recording to become more proactive in your IBS management? As we’ve seen, using a tool like the Bristol Stool Chart can be extremely helpful in knowing what and how to track information relating to your IBS. Start your monitoring practice by simply writing down the ‘type’ numbers of your stools on a daily basis. That way, you can easily average out the scores, or see a range in the numbers, to portray what a typical week looks like when seeing your doctor.
It’s also helpful to score your other IBS symptoms, as a number on a scale of 1 to 5, to indicate their frequency and severity. Again, this makes it easier to track your progress over time and communicate with your doctor. Other things you may wish to track include details of your daily diet, if your sleep is poor or interrupted, how much you exercise, and your overall stress levels each day.
In addition to the Bristol Stool Chart, there are many helpful, freely downloadable resources out there, including printable templates and apps.3,5-9 Some of these even have built-in analytics to help you detect trends and associations between your IBS symptoms and potential triggers. Why not play around with some to see which works best for you?
We hope you feel inspired to go and start tracking your IBS symptoms every day! Just remember to keep everything as simple and concise as possible so that your doctor can easily understand, see the trends, and better support you in your treatment journey.